A team of researchers has utilized organoid technology to cultivate miniature human lacrimal glands capable of producing tears. These organoids serve as models for studying how certain cells in the human lacrimal gland produce tears or fail to do so, aiding in the understanding of the biological characteristics of crying and dry eye disease. While regenerative therapy using human lacrimal gland organoids is unlikely to be realized in the short term, these researchers have demonstrated that organoids can be transplanted into the lacrimal glands of mice, integrating and producing mature tears. This significant achievement was published in the March 16th issue of Cell Stem Cell. Hans Clevers, the corresponding author of the article, stated, "We hope scientists can use our model to test new drugs or expand healthy cells on patients' organoids and one day use them for transplantation to identify new treatment options for patients with lacrimal gland diseases." The lacrimal gland is crucial for lubricating and protecting the eyes. Disorders or dysfunction in tear secretion can lead to dry eye disease or Sjögren's syndrome, a lesser-known autoimmune disease that causes dry eyes and mouth. Current treatment options for patients with lacrimal gland diseases include eye drops, tear duct plugging, and surgery.
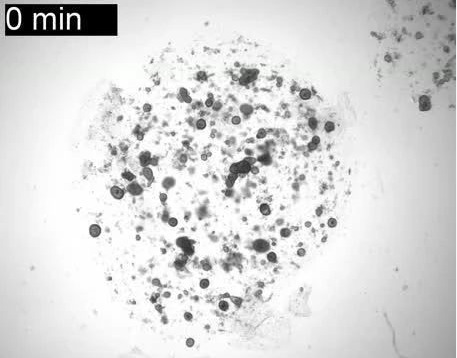
Another author, Yorick Post, added, "To our shock, it is estimated that at least 5% of the adult population suffers from dry eye disease, which in most cases is related to deficiencies in tear production by the lacrimal gland. However, treatment options are limited due to our incomplete understanding of the biology and the lack of reliable long-term in vitro models to study the lacrimal gland." To overcome this obstacle, the researchers generated 3D mouse and human lacrimal gland organoids from adult stem cells using protocols previously used for other organs. The organoids could expand for months and recapitulate the structural, transcriptional, and functional features of lacrimal gland epithelial tissue, including most of the tears secreted by the lacrimal gland epithelial tissue. Notably, the organoids swelled like balloons when exposed to the neurotransmitter norepinephrine, triggering tear secretion. "It was a challenge to get the organoids to cry, as this is a hallmark of the lacrimal gland," said Marie Bannier-Hélaouët, the first author of the article. "We had to modify the combination of factors in which the organoids were grown to make them possess mature cells in the lacrimal gland that could cry." The researchers used mouse organoids to study the role of Pax6 (a major control gene for eye development) in the adult lacrimal gland. By deleting Pax6 using CRISPR-Cas9 genome editing, they found that this gene is important for the maturation of adult lacrimal gland epithelial cells. These special organoids could provide valuable insights into potential treatments for Sjögren's syndrome, as PAX6 deficiency has been observed in the eye tissue of these patients. The researchers also used single-cell mRNA sequencing to analyze the cellular characteristics and the origin of tear components in the lacrimal gland. Their single-cell atlas revealed new tear components and showed that duct and acinar cells in the human lacrimal gland secrete different tear components. To test the potential of organoids in regenerative medicine, the researchers then transplanted human organoid cells into the lacrimal glands of mice. Two weeks later, the human organoid cells formed ductal structures and persisted in the lacrimal gland for at least two months. The implanted organoids seemed to be self-organizing, and some cells were proliferating two months after transplantation. In addition, the researchers detected tear proteins within the ducts formed by the transplanted cells.
The beneficial effects of organoid transplantation will need to be validated in mouse models of dry eye disease. Future research could also focus on modeling Sjögren's syndrome by integrating immune cells into the organoids. Clevers said, "Patient-derived organoids open up new avenues for studying lacrimal gland diseases in a personalized way. However, there is still a long way to go before using these miniature organic mimics for regenerative therapy."
Reference:
Exploring the human lacrimal gland using organoids and single-cell sequencing